Addressing Inequalities: Structural Competency and Collective Action in Mental Health
There have been multiple engagements with the dominant bio-medical discourse in mental health, whether it is the need to center psychosocial interventions or to re-conceptualise a treatment gap as a mental health care gap as well as human rights violations, a lack of patient-centered approaches and policy gaps. While the focus on supply-demand issues in mental health services has insidiously rendered the invisibility of mental health as a global challenge and a development issue, the latter’s structural underpinnings of social, political and economic identities remain unaddressed. How does this neglected aspect of mental health inequality, its perpetuating causes interact with and evaluate the clarion calls for more and better quality services, data and research as well as increased funding?
The scope of this essay is to understand both; the narratives of mental well-being through the socio-political forces that create them, as well as how larger systems of power impact phenomenological experiences. The structural analysis shared here will further direct the goals of mental health systems and advocacy efforts towards the pursuit of health equities, and subsequently, social justice.
This socio-political lens allows us to situate mental health within people's lives, experiences and contexts. It helps us recognize that marginalized individuals may be disproportionately impacted by mental health concerns, in part due to a greater exposure to stressful events and a lack of social support. Exacerbating this, is the fact that the same mechanism of systemic oppression influences who provides mental health services, who is able to access them, and who these services are designed for. In fact, it is the same oppressive structures that govern public policy and sociocultural norms - be it health, social or economic. And the combination of these factors come together and perpetuate inequalities in mental health.
Thus, it’s necessary to ask questions about the gaps in mental health service, data, and funding, as well as those in social safety nets, policies, and laws. Importantly, we also need to study the factors that influence the distribution of social, economic and physical resources, which in turn influence disparities in mental health outcomes. To work toward health, justice, and equity, we must understand how structural determinants are deployed at a population or systems level, community level, clinical level and individual level.
Reframe aims to explore the roots of these determinants lying outside the therapy rooms and randomized control trials - in policies, in public and private institutions such as schools, workplaces, media, families, communities, in social narratives, in mental health advocacy and bigotry of the healthcare systems themselves. Be it youth mental health, suicide prevention or stigma - it is evident that they require multi-sectoral efforts (across government departments, workspaces, educational spaces, media, as well as in communities and families). However, what we need to realise is that the efficacy of such multi-sectoral interventions will depend on how they address the root causes that lie on the axes of caste, gender, class, ability, sexuality and ethnicity.
Can we talk of youth mental health without considering the effects of one’s future being decided by solitary competitive exams, or of institutionalized casteism in entrance exams, or of the lack of sexual and reproductive health rights?
The individualist way of analyzing mental distress requires criticism of another aspect of contemporary mental health advocacy: The dismissal of structural backdrops behind pain, anxiety, mourning and other psychological experiences. To acknowledge the social construction of the terminologies of mental distress is not to deny the experience of distress but instead to relocate the origin of it in structural forces such as casteism or cis-heterosexuality. As such, the scope of this Reframe issue is to explore, deconstruct, and deny the illusionary location of distress within a private realm, isolated from social systems such as politics, economy, society, communities, policies, and identity.
Additionally, one has to consider concrete steps to dismantle the ways in which casteism, patriarchy, religious discrimination, and ableism have been institutionalized in healthcare systems themselves. Without addressing the inbuilt discrimination in mental health approaches, curricula and practice, we cannot hope to resolve unequal access to care either.
Systems born of inequalities cannot bring about change
The reforms in psy-disciplines have focused on challenging the legacy of the asylum, profit-making, and pharma. This has led to the assertion of user-survivor voices. However, simply this assertion is not enough because it stops short of dismantling the systems of power that reflect social hierarchy, and built and reinforced the psy-disciplines in the first place.
If we use the lens of systems of power, and of privilege and oppression, it will enable us to contest the definitions and visible narratives of mental health. For example, why is workplace mental health centered around white-collar spaces? And, are persons with visual, locomotor or aural disabilities considered when planning mental health services?
In South Asia - ability, caste, class, ethnicity, gender, sexuality, and religion play a pivotal role in determining the daily stressors, exposures, and susceptibility to mental ill-health. They also inform the options for recourse one can access - in terms of both, mental health support and wider supports such as social safety nets, as well as the quality of care and support received. All major public and social institutions are also entrenched in these forces of oppression and collude to uphold their order in both norms and policy. These oppressions and their consequences therefore interlock, exacerbate, and perpetuate the situation for those who are marginalized, creating a vicious cycle.
Changes in legal and social policy are pivotal in addressing mental health inequalities by mitigating risk and increasing protective factors in multiple contexts - workplaces, education, legal systems etc. While social change is critical towards building health equity - it being a long term process, necessitates policy changes to precede cultural change.
Multi-dimensional Poverty
A 2021 study by Azim Premji University found that 230 million Indians were pushed into poverty after one year of COVID-19 leading to widespread unemployment, loss of income, food insecurity and homelessness. Food insecurity is a risk factor for both mental and physical health. Apart from the immediate result of undernutrition, it results in unrelenting distress, anxiety, shame, powerlessness and guilt. Consequently, food deprivation is linked to a higher probability of non-communicable diseases such as diabetes and cardiovascular disease as well as depression and anxiety. This is accompanied with an increase in health care costs and shares a bidirectional relationship with poverty.
Similarly, there are inter linkages between poverty, homelessness, and mental illness. While being homeless places an individual at an increased risk of developing mental illness, there is also an increased risk for becoming homeless due to mental illness. The likelihood of living with mental illness is three times greater for homeless persons as compared to the general population. The psychological dimensions to homelessness - high levels of stress, uncertainty and anxiety - are exacerbated by greater exposure to violence (from individuals and the state), unemployment, lack of access to education and adverse childhood experiences.
Women who are left behind
Using the lens of structural determinants tells us that women who face homelessness are more vulnerable to sexual assault and gender based violence (GBV). Those who experience GBV may experience depression, anxiety, stigma, shame and are at an increased risk for mental health conditions. However, looking along the fault lines of caste, gender and ability, we see that more often than not, trans women, dalit women, adivasi women, sex workers and women with disabilities are not included in the definition of ‘women’.
If we unpack some of these examples, we can better understand how multiple marginalizations interact with each other.
Casteism
Take for example, the fact that five out of six multidimensionally poor people in India are from Dalit, Adivasi or Other Backward Class (OBC) families. Further, over one-third of homeless persons are Dalits, showing that the intergenerational cycle of social discrimination and exploitation is profoundly linked to poverty. Unless we use a structural lens, our systems and policies will also miss structural exclusion from social safety nets.
Transmisia
Trans persons living in poverty face unique challenges. A study conducted in urban India and Brazil found that trans women had a lack of employment options and job security. Apart from the stigma of poverty they also faced social isolation due to entrenched prejudice, discrimination, and gendered violence, which then intensified their mental health concerns such as suicidal ideation. Since social safety nets largely require formal identification - they’re likely to be inaccessible for trans persons. This is also true for Dalit persons who are homeless - a study found that despite having identification, almost no Dalit persons were able to access benefits such as as subsidized food ration. Thus, for any policy measure against malnutrition, homelessness, or poverty to be effective, the intergenerational cycle of discrimination, exploitation, and exclusion due to caste must be addressed specifically, and must also vary for measures addressing trans issues, and disability rights.
Clearly, individuals from different contexts experience varied dimensions of discrimination - which are linked to posttraumatic stress, depression, and generalized anxiety disorder among other mental health conditions. Such discrimination or perceived discrimation can have a knock on effect leading to limited access to health care, employment, and housing. Here, it is important to also point out that discrimination is embedded in health care systems themselves - whether it is Dalit persons being barred from entering health-care centers, doctors not touching Dalit patients, or LGBTQIA+ persons facing forced pathologization, ‘treatment’, incarceration, and ‘cure’.
Islamophobia
To explain, a cycle of exclusion, protest and violent suppression creates yet another generation of children and adults who internalize their marginalization, accepting discrimination at workplaces, in colleges, or in public spaces inevitable cost to be paid. When islamophobic narratives create dehumanizing policy, violence, microaggression, and deny economic sufficiency, land and social security, the psyche of Indian muslims cannot be explored in isolation. “Self esteem” here, cannot be defined as an individual’s appraisal of themselves as if the actual evidence of hate they are receiving in their lives is not contributing to this self perception. “Anxiety” for muslim women arises out of an actual threat of sexual violence they are vulnerable to because of the intersections of patriarchy and islamophobia. When the prerequisites of psychological health are gatekept by structural forces of casteist exclusion, heteronormative and political violence, ableist narratives and capitalist policy, mental health empowerment is to root in the altering of these narratives, change in policy, social relations and livelihood security.
Other than institutionalized discrimination - the above examples also speak to active perpetuation of stigma. However, in mental health stigma is almost exclusively viewed as individual or interpersonal, rather than structural. Based on the above examples, it is clear that we need to approach stigma structurally. This would mean stepping away from ‘awareness campaigns’ and linear recovery narratives, and working to actively trace the pathways that stigma takes.
Rethinking research and advocacy
A structural approach would inform which voices of lived experience matter, and would include not only those who have experienced incarceration in a mental health institution, or who have been prescribed medication, but a much wider range of people who have experienced stigma. This also points to the need to challenge stigma as a narrow interpersonal or social phenomenon, and look at it as something that resides in multiple contexts. As Bolster-Foucalt et al outline, stigma exists in “legal frameworks, welfare policies, economic policies, social and built environments, media and marketing, pedagogical factors, health care policies and practices, biomedical technology, diagnostic frameworks and public health interventions.
Using the lens of structural determinants would also affect approaches to research and advocacy in mental health. For example, a research study by Hatzenbuehler et al found in 2004 that LGB adults who lived in areas that banned same-sex marriage experienced significant increases in mood disorders, alcohol dependency, and in generalized anxiety disorders, versus LGB adults who lived in areas without marriage bans. In another study Hatzenbuehler et al found the first state in the USA to pass a same-sex marriage law saw improvements in the health of gay men with significant reductions in depression, hypertension and stress disorders, all within 12 months of the law being passed. This can allow one to posit that affirmative policies addressing structural forms of stigma may improve health indicators, whereas institutional, policy and law based stigma can negatively impact health indicators.
While policy changes may have significant effects, there also need to be commensurate changes within health structures. Despite the repeal of Section 377 in India and the National Legal Services Authority (NALSA) 2012 judgement, structural stigma resides in mental health curricula and in practice both - with LGBTQIA persons being forced to undergo conversion treatments and more. Both psy-disciplines and physical health - are grounded in biological explanations or cultural differences related to health behaviours. Neither of these approaches foreground structural causes that limit and impact individual well-being. Thus, all curricula need to be reformulated for structural competency - recognizing, understanding and addressing the structural determinants that shape patients’ health and create health inequities.
Structural Competency
Developing medical or psychiatric expertise has been largely restricted to the biological and cultural lens so as to individualise ‘health-related behaviours’ such as substance dependency. To provide acceptable and appropriate services to all, it is clear that the services must be affirmative i.e. able to recognize and address the effects of structural oppression that lead to a range of inequalities.
However, the psy-disciplines - by virtue of defining what is ‘normal’ and ‘abnormal’ - are one of the key pivots for structural oppression around ability and neurotypicality. This difference is politicized when it is unequally catered to, where some minds are normalized while others are pathologized. This occurs through creation of economic policies, political systems, familial norms, and community standards that accommodate and fulfill the needs of few people who then enjoy the power of a socially constructed, exclusionary and rigid notion of “normal mind.”
People with mental illnesses and neurodivergence who lie outside this construct are marginalized by this system of neurotypicality. For example, educational curriculums, timelines and deadlines don't cater for the needs of students with autism; and the ambitious glorification of work and hustle dehumanizes people with anxiety, depression, psychosis and other mental illnesses who do not fit the ableist expectations. In addition, mental health campaigns depict linear recovery narratives - thereby upholding neurotypicality as the desired, default, and successful destination to reach. To look structurally at ‘illnesses' ' is to also understand and resist the systems that define them as medical ‘issues’ and the stripping of agency, individualized responsibility and isolation brought by the endowment of pathology.
A “mental disorder” is currently in the vocabulary of deficits. The “lack of emotional expressions,” “the lack of behavioural participation,” “the lack of productive labour” are phrases that can be found as symptoms of mental illnesses in diagnostics bibles. The deficits are measured against a pre-existing expectation of what is normal and the deviance is hence defined as abnormal. The diagnostic claims made by a psychiatrist are hence, essential ethical judgements regarding the congruence of one’s behavioural expression with that of social expectations. This signifies that mental health is not a matter of natural phenomenons but socially constructed taxonomies of illness and recovery.
What are the nuances of such narratives of normalcy, who constructs them and what consequences the labels bring then become important. Hysteria was popularly used as a term to define women who presented themselves differently than the white man’s criteria for a normal woman. Gender dysphoria, a term explaining an experience caused when one is denied agency over and acceptance for their gender is termed as a mental disorder. Autism and ADHD, representing a diverse expression of the human mind, are defined as learning disorders. The pattern implies the construction of “disorders” to be non-conformity of social norms or the inability to function and participate in such a society due to the said norms. Hence at the very basic stage of semantics, mental disorders are often socially constructed labels for certain experiences, determined by structural forces.
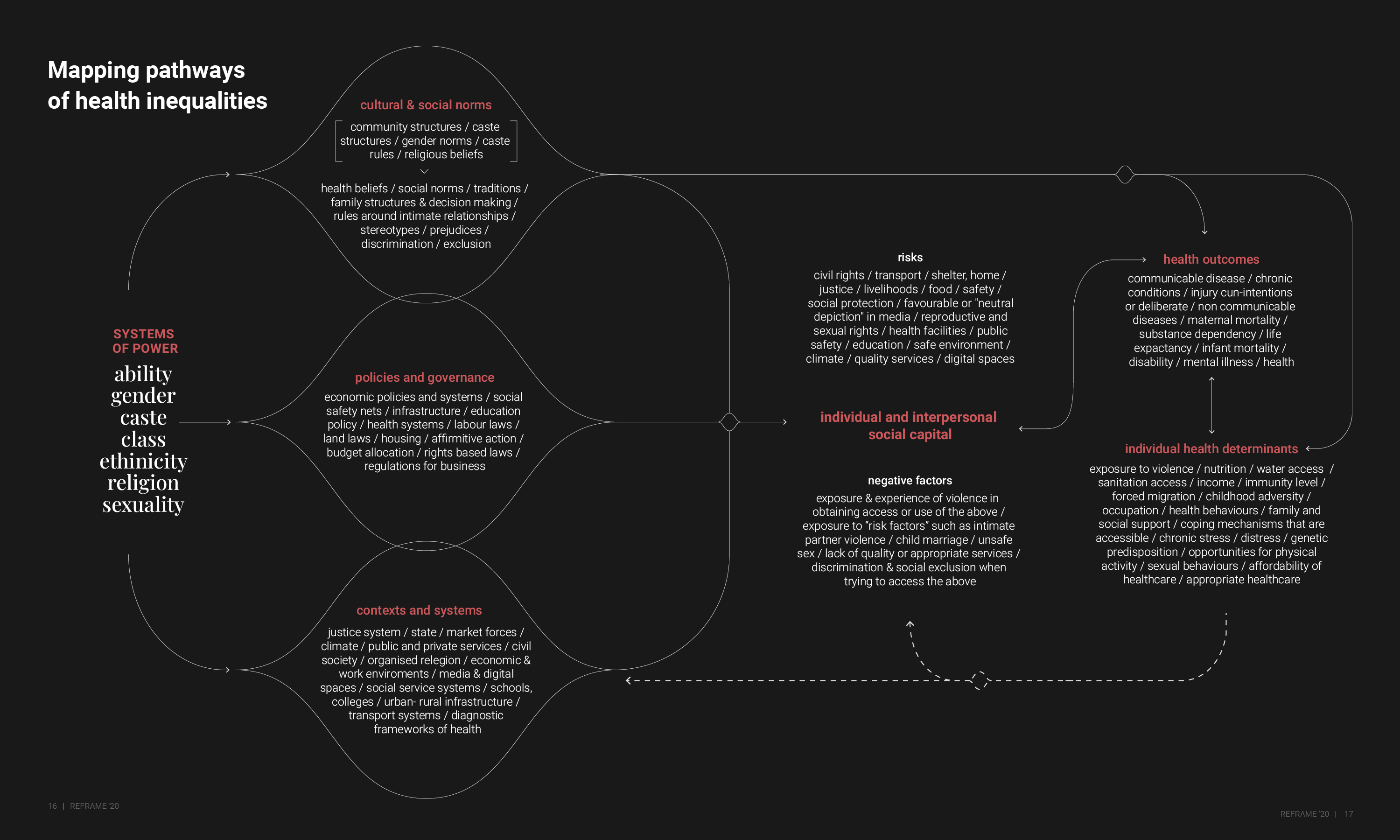
Mapping pathways of health inequality
Mental health is political
An integral part of building structural competency is learning from lived realities and centering the knowledge and labour of the margins. This cannot be done without the involvement of persons who are marginalized by structural oppression.
Further, to build structural competency within the psy-disciplines, the complicity of mental health must be acknowledged and subsequently countered with the understanding that responsibilities extend beyond the therapy room or simple service provision. This legacy of structural violence and discrimination in mental health must be challenged in multiple ways.
To paraphrase a report on ‘Building Allyship’, mental health practitioners or systems must take it upon themselves to provide psychoeducation to multiple stakeholders who hold power - whether it be families or neighbourhoods, courts, educational institutions, media etc. This must include building a supportive network of structurally competent allied services and practitioners. It is imperative for mental health practitioners to deploy the privilege of their expertise to testify for courts, and for policymakers to push reforms that will affect health equity - whether for welfare benefits, workplace safety or affirmative action policies.
This will also necessitate a commitment to collective politics, communication, allyship and solidarity between mental health and activist movements such as women’s rights movements, anti-caste movements, disability rights, labour rights, LGBTQIA+ and black lives matter. We cannot side-step the need to address social, economic and institutional exclusion that contributes to psychosocial distress - which means widening our ambit beyond affirmative mental health policy and services to demand freedom from violence and food insecurity, as well as better provisions of social safety nets, labour rights, lgbtqia+ rights and human rights.
Click here to download the full version of ReFrame IV
_______________________________________________________________________________
“This also points to the need to challenge stigma as a narrow interpersonal or social phenomenon, and look at it as something that resides in multiple contexts.”
References
(1) Pathare, Soumitra, and Jasmine Kalha. “Pathways to Mental Health.” ReFrame: Bridging The Care Gap, vol. 2, 2019, pp. 4–9.
(2) Kohli Dave, Amalina, and Raj Mariwala. “Clinical Legacies and Counter-Narratives.” ReFrame: Beyond Clinical Contexts, vol. 3, Sept. 2020, pp. 3–12.
(3) McAllister, A., et al. “How Do Macro-Level Structural Determinants Affect Inequalities in Mental Health? – A Systematic Review of the Literature.” International Journal for Equity in Health, vol. 17, no. 1, 2018. Crossref, doi:10.1186/s12939-018-0879-9.
(4) Lorant, V. “Socioeconomic Inequalities in Depression: A Meta-Analysis.” American Journal of Epidemiology, vol. 157, no. 2, 2003, pp. 98–112. Crossref, doi:10.1093/aje/kwf182.
(5) Kohli Dave, Amalina, and Raj Mariwala. “Today’s Landscape.” ReFrame: Funding Mental Health, vol. 1, Sept. 2018, pp. 7–10.
(6) Solar, O, and A Irwin. World Health Organization, Geneva, Switzerland, 2010, pp. 3–62, A Conceptual Framework for Action on the Social Determinants of Health, www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf. Accessed Oct. 2021.
(7) Kohli Dave, Amalina, and Raj Mariwala. “Clinical Legacies and Counter-Narratives.” ReFrame: Beyond Clinical Contexts, vol. 3, Sept. 2020, pp. 3–12.
(8) Basole, Amit, et al. Azim Premji University, Bengaluru, Karnataka, 2021, pp. 1–234, State of Working India 2021: One Year of Covid-19. https://cse.azimpremjiuniversity.edu.in/wp-content/uploads/2021/05/State_of_Working_India_2021-One_year_of_Covid-19.pdf . Accessed November 2021.
(9) Bhargava, Ruma, and Megha Bhargava. “Covid-19 Is Creating a Hunger Catastrophe in India – Here's an Opportunity to Break the Cycle.” COVID-19 Is Creating a Hunger Catastrophe in India – Here's an Opportunity to Break the Cycle, World Economic Forum, 15 June 2021, https://www.weforum.org/agenda/2021/06/covid-19-pandemic-hunger-catastrophe-india-poverty-food-insecurity-relief/. Accessed November 2021.
(10) Jones, Andrew D. “Food Insecurity and Mental Health Status: A Global Analysis of 149 Countries.” American Journal of Preventive Medicine, vol. 53, no. 2, 2017, pp. 264–273., https://doi.org/10.1016/j.amepre.2017.04.008.
(11) McGuire, Shelley. “Comprehensive Implementation Plan on Maternal, Infant, and Young Child Nutrition.” Advances in Nutrition, vol. 6, no. 1, 2015, pp. 134–135., https://doi.org/10.3945/an.114.007781.
(12) Siddiqui, Faareha, et al. “The Intertwined Relationship between Malnutrition and Poverty.” Frontiers in Public Health, vol. 8, 2020, https://doi.org/10.3389/fpubh.2020.00453.
(13) Funk, Michelle, et al. “Mental Health, Poverty and Development.” Journal of Public Mental Health, vol. 11, no. 4, 2012, pp. 166–185., https://doi.org/10.1108/17465721211289356.
(14) World Health Organization, et al. 2013, pp. 1–51, Global and Regional Estimates of Violence against Women.
(15) Oxford Poverty and Human Development Initiative, United Nations Development Program, 2021, pp. 1–41, Global Multidimensional Poverty Index 2021.
(16) “A Homelessness Study Whose Findings Should Unsettle Us.” The Telegraph, 16 Oct. 2019, https://www.telegraphindia.com/opinion/a-homelessness-study-whose-findings-should-unsettle-us/cid/1712170. Accessed Oct. 2021.
(17) Gomes de Jesus, Jaqueline, et al. “Mental Health and Challenges of Transgender Women: A Qualitative Study in Brazil and India.” International Journal of Transgender Health, vol. 21, no. 4, 2020, pp. 418–430., https://doi.org/10.1080/26895269.2020.1761923.
(18) “A Homelessness Study Whose Findings Should Unsettle Us.” The Telegraph, 16 Oct. 2019, https://www.telegraphindia.com/opinion/a-homelessness-study-whose-findings-should-unsettle-us/cid/1712170. Accessed Oct. 2021.
(19) Williams, David R., and Selina A. Mohammed. “Discrimination and Racial Disparities in Health: Evidence and Needed Research.” Journal of Behavioral Medicine, vol. 32, no. 1, 2008, pp. 20–47., https://doi.org/10.1007/s10865-008-9185-0.
(20) George, Sobin. “Caste and Care: Is Indian Healthcare Delivery System Favourable for Dalits?” 2015, https://doi.org/https://ideas.repec.org/p/sch/wpaper/350.html. Accessed Oct. 2021.
(21) Sharma, Prateek. “When Bigotry Invades Mental Healthcare: Women, Sexual Minorities Are Most Vulnerable to Harassment.” Scroll.in, 1 Nov. 2016, https://scroll.in/pulse/820412/when-bigotry-invades-mental-healthcare-women-sexual-minorities-are-most-vulnerable-to-harassment. Accessed Nov. 2021.
(22) Kohli Dave, Amalina, and Raj Mariwala. “Clinical Legacies and Counter-Narratives.” ReFrame: Beyond Clinical Contexts, vol. 3, Sept. 2020, pp. 3–12.
(23) Bolster-Foucault, Claire, et al. “Structural Determinants of Stigma across Health and Social Conditions: A Rapid Review and Conceptual Framework to Guide Future Research and Intervention.” Health Promotion and Chronic Disease Prevention in Canada, vol. 41, no. 3, 2021, pp. 85–115., https://doi.org/10.24095/hpcdp.41.3.03.
(24) Hatzenbuehler, Mark L., et al. “State-Level Policies and Psychiatric Morbidity in Lesbian, Gay, and Bisexual Populations.” American Journal of Public Health, vol. 99, no. 12, 2009, pp. 2275–2281., https://doi.org/10.2105/ajph.2008.153510.
(25) Hatzenbuehler, Mark L., et al. “Effect of Same-Sex Marriage Laws on Health Care Use and Expenditures in Sexual Minority Men: A Quasi-Natural Experiment.” American Journal of Public Health, vol. 102, no. 2, 2012, pp. 285–291., https://doi.org/10.2105/ajph.2011.300382.
(26) Supreme Court of India. NATIONAL LEGAL SERVICES AUTHORITY (NALSA) VS. UNION OF INDIA. South Asian Translaw Database, https://translaw.clpr.org.in/case-law/nalsa-third-gender-identity/. Accessed Oct. 2021.
(27) Metzl, Jonathan, and Dorothy Roberts. “Structural Competency Meets Structural Racism: Race, Politics, and the Structure of Medical Knowledge.” AMA Journal of Ethics, vol. 16, no. 9, 1 Sept. 2014, pp. 674–690., https://doi.org/10.1001/virtualmentor.2014.16.9.spec1-1409. Accessed Nov. 2021.
(28) Hansen, Helena, and Jonathan M. Metzl. Structural Competency in Mental Health and Medicine a Case-Based Approach to Treating the Social Determinants of Health. Springer, 2019.
(29) Szasz, Thomas. “The Myth of Mental Illness.” Biomedical Ethics and the Law, 1976, pp. 121–130., https://doi.org/10.1007/978-1-4684-2223-8_10.
(30) Chakravarty, Shruti, and Aashima Sodhi. Mariwala Health Initiative, Mumbai, Maharashtra, 2021, pp. 1–50, Building Allyship: The Mental Health Community and LGBTQI+ Rights, https://mhi.org.in/media/insight_files/Building_Allyship.pdf. Accessed Oct. 2021.