Unrecognized and Unaddressed
The mental health of persons with disabilities
trauma of an ableist world
“Survival of the fittest” was not just a Darwinian theory in our 6th Std school textbooks; over the years, we observe that it is a concept in which the majority believes. What then happens to those who are considered unfit – defective, less, disabled? Not many people might call you “defective” to your face if you live with a disability, but the raised brows, the "hmm"s, the discomfort that nondisabled persons exhibit, and the inaccessibilities they encourage and perpetuate, speak volumes to the person with a disability.
The constant subtext in the messages that surround persons with disabilities (PWDs) is that they are not worthy, they are incapable, they are a burden, and they are not needed. Just like the trees in the Solomon Islands that are popularly believed to die – and thus become easier to cut down – when cursed, many PWDs succumb to the negative messaging and start doubting themselves. Some of them become convinced that they are somehow lesser beings, forced into dependence, and begin feeling “not normal” all the time. On the other hand, some PWDs, as a defence mechanism, fake ableist independence, or almost kill themselves trying to prove to the non-disabled world that they can overcome whatever hurdles are thrown at them, because they are expected to be superhumans and are under a scanner all the time.
Imagine a life where judgments and conclusions about you are arrived at with just a glance (in cases of visible disability), or you are disbelieved, even suspected to be lying (in cases of invisible disabilities). PWDs live with this trauma. They are constantly questioned, prohibited or only reluctantly “allowed” by nondisabled society to do “normal” things that others take for granted, like education, access to public spaces, socializing, work, relationships, marriage, and so on. Discrimination is a constant, with abuse and violence not far away. In such an environment, many PWDs tend to internalize the stigma and behaviors they encounter. These realities shape the conversation around PWDs, which is generally couched in terms of their basic survival, rather than of their right to live their lives to the fullest.
PWDs are not a homogenous group. Individual experiences differ, depending on factors such as the nature of the disability, and privileges or otherwise of location, gender, etc. There is one significant difference – that between congenital (born disabled) and acquired (late disabled through accidents, disorders etc.) disability. In both situations, similar discriminations and difficulties prevail, but in the case of an acquired disability the individual themselves may carry an ableist mindset as they transition from one world to another. They may have predetermined notions about their life, potential, and future, which are not grounded in fact but rooted in stereotypes. So most often when people acquire their disability, the first thing they believe is that life cannot be lived with blindness, deafness and so on. They believe they would not be able to work, they won’t be fit for social participation etc., all based on ignorance and access to stigmatized messaging and information when they were non-disabled.
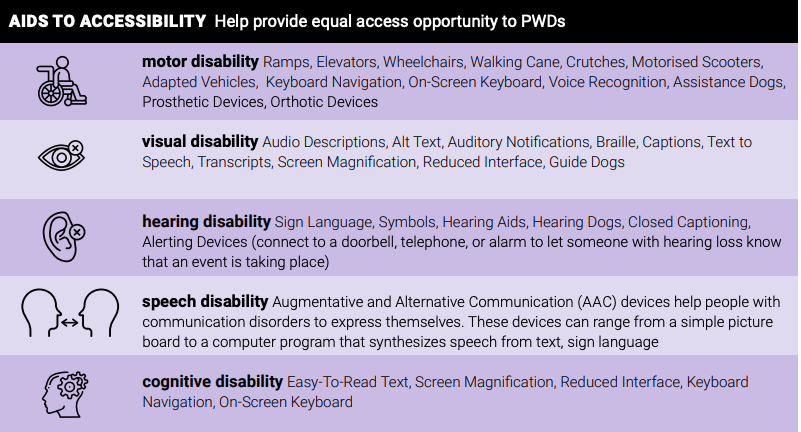
AIDS TO ACCESSIBILITY Help provide equal access opportunity to PWDs
mental health gap for persons with physical and/or sensory disabilities
So what happens when you are disabled? Disability is generally viewed through the medical lens of disease, and correction. For those with a physical/sensory disability, some medical rehabilitation, however imperfect, is usually possible. However, what is neither routinely recommended nor provided is any kind of mental health rehabilitation and support. This extremely important need is hardly recognized. Most problems that PWDs face tend to be attributed to their disabilities. So if they don’t get admission in an institute or face challenges there, it is not because of lack of reasonable accommodation, it is because of their disability is what is told to them; when a disabled woman is harassed while seeking assistance she is told that it is because she is disabled and needs help. Discrimination and abuse add their own weight to the already present guilt and shame many PWDs experience. Traumatic experiences accompany being disabled almost like a package deal, and this not only normalizes the trauma, it prevents the PWD from speaking out against it or seeking external help to cope with it.
Mental health and physical disability together form a difficult intersection, both being highly stigmatized. This intersection is seldom recognized, and rarely discussed. The idea persists that PWD are disabled, not “mad”, and therefore do not require mental health support. This view serves only to perpetuate the stigma around mental health concerns, and makes it extremely challenging for PWDs to access mental health care.
Access barriers exist at multiple levels. To begin with, many PWDs need mobility and transport assistance, which is provided (if at all) mainly by family members. As a consequence, the PWD rarely has privacy in interactions with counselors or therapists or doctors. This becomes particularly complex when the trauma inflictors are the family members themselves. If the PWD is deaf or has other hearing or speech impairments, they have to take along an interpreter because almost no medical practitioners know sign language. Additionally, the clinics or centers may not be physically accessible.
The bigger barriers are the intangible ones. Training and sensitizing about the needs and concerns of PWD are not a part of medical or counseling curricula. Most practitioners, then, come with the popular ableist and stereotyped beliefs about disabled persons. Many might never have interacted with a single disabled person in their entire lives and careers. PWDs are routinely infantilized, which means that in most cases they are not directly addressed, or believed – the counselors or doctors talk to or question their family members, instead. Such an approach strips PWDs of their agency; obtaining consent from a disabled person gets reduced to a formality and is rarely real, informed consent.
Therapists who cannot unravel these several layers often do more harm than good. They may even end up suggesting coping techniques that are ableist, and better suited to non-disabled persons, or in other words, better suited to fit into the nondisabled/ableist world.
Living with a disability is not easy, particularly in the current environment of inaccessibility. The gaps in physical care are visible and substantial. But the void in mental health care and support is invisible, and unrecognized. The impact of this care gap is immense, allowing an entire community to remain mired in guilt, shame, low self-esteem, too often with under-utilized personal potential – just surviving, rather than living life to its fullest
“None”
