Long form: Clinical Legacies and Counter-Narratives
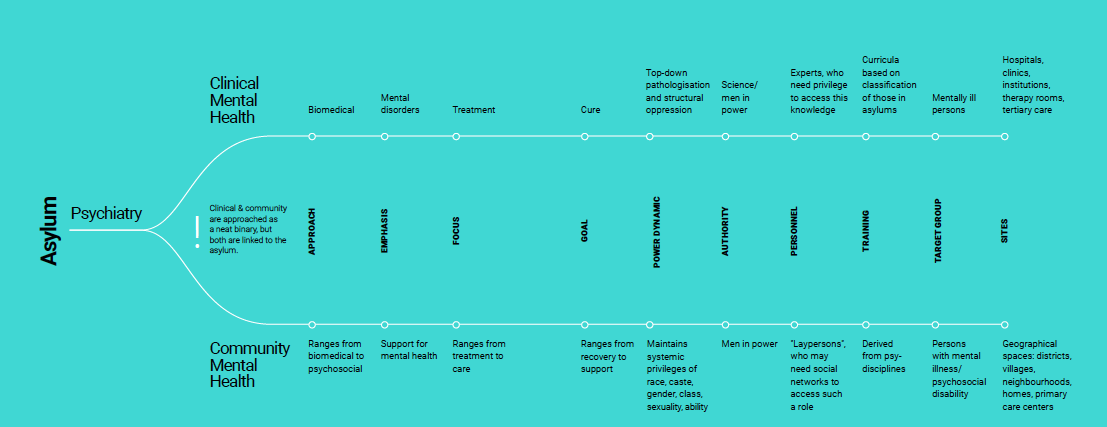
The fields of knowledge associated with mental health have come under scrutiny for human rights violations, incarceration, their lack of patient-centered approaches, an over-emphasis on productivity, and ethical concerns around pharmacology. In this piece, we will look at the history of psy-disciplines and trace a trajectory to alternatives such as community-based mental health.[1] Although social inclusion together with community mental health care are perceived as a panacea of sorts for dealing with oppression by psy-disciplines, the “community” cannot be assumed to be a caring monolith, nor may we presume that mainstream communities do not reflect the heritage of the clinical. To explore the ways in which we can move away from replicating the oppression in psy-disciplines, we must look toward histories of practice, and strive to learn from marginalized communities.
The asylum
The history of modern psy-disciplines is firmly rooted in the spaces called “asylums”, as well as in hospitals and clinical institutions.[2] The idea of earmarking a space for the containment of distress has many examples in history – one of the earliest being Bethlem Royal Hospital (the origin of the term “bedlam”) founded in 1247, and then widespread through Europe in the 16th and 17th centuries.
Interestingly, there were both public and private institutions, providing treatment or incarceration of those deemed unmanageable by their families, or “insane”.[3] This categorization included persons who lived in poverty, undertook sex work, had physical disabilities, or were seen as grossly “immoral”.[4] Authors Arnold and Scull speak of how unmarried pregnant women, persons disloyal to the regime of the time, and people suffering from epilepsy were also incarcerated. Individuals from wealthy families, or those with adequate personal means, were remanded in private institutions with relatively comfortable living conditions.
While private asylums were profitable enterprises, public or religious charitable institutions were divided up into the asylum, the prison, and the workhouse. Thus, there sprung up terms of separation such as “criminal lunatics” and pauper lunatics. Institutions like these paved the way for the idea that special, separate spaces were necessary to treat and confine those who did not conform to societal standards of behaviour, or were seen as failing to participate in economic systems.
The confinement and silencing of individuals began as social disciplining tools, given that these spaces were not necessarily run by trained doctors or experts but by interested persons such as priests and physicians, even entrepreneurs.[5] The power relations between patients on the one hand, and caretakers or “experts” on the other, were clearly demarcated and strictly enforced in these spaces – with patients being restrained with chains, straitjackets and other forms of coercion, ostensibly to prevent “antisocial behaviour” or self-harm. This form of custody often required violent enforcement.[6]
Defining normal and mad
Asylums further allowed for the study of behaviour that was seen as “abnormal” or unproductive, and of distress and madness as individual, personal phenomena. It was in these spaces that the building of psychiatric and psychological knowledge began.[7] In this manner, asylums gave birth to the system of knowledge we call psychiatry – which soon had the monopoly on definitions of both “normal” and ”mad”. And they gave the men in charge (almost never women), the self-fashioned experts, opportunities to experiment with and administer treatments devised by themselves to control and to “cure” incarcerated persons. Seclusion, for instance, was supposed to help a person regain sanity, and corporal punishment was believed to cure certain mental illnesses.[8] A number of early mental health treatments seem to have been rooted in the idea of punishment.
In this history, then, lie the roots of the idea that mental illness is violent and dangerous, something to be frightened of, and that it therefore requires that those afflicted by it be excluded from the mainstream, and punished. By the late Victorian period, theories around the biological as well as hereditary nature of madness were becoming popular.[9] This type of biological and medical framing of the discourse contributed to the idea of psychiatry as neutral, objective, and scientific, while heightening power differentials through the increasing specialization and professionalization of the study of mental illness.
Building diagnoses
The colonialist propagation of this system is evident from the establishment, between 1787 and 1795, of India’s first asylums in Calcutta, Kilpauk and Munger, where patients diagnosed as mentally ill were secluded away from mainstream society.[10]
Soon after, in 1805, Jean-Étienne Dominique Esquirol published ‘The passions considered as causes, symptoms and means of cure in cases of insanity’. This was the first attempt at classifying mental illnesses, deriving from his own intensive observations and study at the asylum he had founded in Paris. Esquirol also drafted the ‘Law of June 30th, 1838’, the first of its kind on the rights of the mentally ill.[11] This French law was later used as the basis for laws in many other countries. In fact, Britain introduced the Lunacy Act (1858) that incorporated guidelines for establishing asylums and admitting inmates, all under the charge of the Inspector General of Police.[12]
In 1883, Emil Kraepelin, generally considered a pioneer of psychiatry, published his ‘Compendium der Psychiatrie’, a classification of mental illnesses based on his clinical observations of patients in German asylums. In this text, he introduced the terms schizophrenia, manic-depressive psychosis, and paranoia. The mirroring of the socio-political prejudices of his age is clear from his theories about the genetics of psychiatric disorders in Jewish people; he also proclaimed that both, opponents of World War I and socialists, were mentally ill.[13] Kraepelin’s classification system became the basis for the Diagnostic and Statistical Manual of Mental Disorders series (DSM), and also for the International Classification of Diseases (ICD).[14]
Morality, profit-making, pharma
The 19th century also saw the advent of an alternative approach: “moral treatment”, which propounded that patients would benefit from being treated humanely – just like other, regular people. Patients were expected to behave in accordance with social norms, eat and talk politely, as well as carry out everyday tasks.[15] The clinical focus shifted to the individual, in whom rational behaviour was encouraged using rules, rewards, punishment and supervision.[16] Restraining methods and physical punishments were relied on less widely.
Around the same time, the stigma around asylums had grown, so much so that the affluent began to send family members to asylums abroad or to nursing homes and sanatoriums in spa towns to avoid their being labelled “insane”.[17] The scope of psychiatry was also broadening, to include more categories of illness – milder disorders such as “nerves”, “neuroses”, “English maladies” – that did not require confinement to mental institutions.
In this manner, lucrative private practice, clinics and facilities began to appear for “curable” patients as well as for those who were to be institutionalized for long periods. More commonly, however, large hospitals were built by the state in large parts of the Western world – providing treatment, work and stable housing for patients. Even as the aim of secluding those with mental illness or other chronic illnesses, as well as the poor and the non-normative, remained implicit, asylums continued to be violent spaces of incarceration due to overcrowding, lack of funds, and the use of methods such as electro-convulsive therapy (ECT) and insulin treatment.[18]
By the mid-20th century, the advent of psychopharmacology, dwindling government budgets, and protests against human rights abuses in asylums were beginning to encourage a process of deinstitutionalization – of replacing long-stay psychiatric hospitals with less isolated community mental health services.[19] This movement took root in many parts of the world, based on the premise that those who required psychiatric treatment would enjoy a higher quality of life and have better chances of recovery if treated in their own communities rather than through leading isolated lives in overcrowded mental institutions.”[20]
community mental health
One of the premises of deinstitutionalization, and the subsequent shift to community MH, is that people can recover from illness when support services function in tandem with the sustenance and stability of families, social networks, and communities.[21] Coinciding with activism from user-survivors of mental health, the deinstitutionalization narrative rings with notes of liberation, human rights, and ethical user-centered care.[22]
However, many lived experiences of community MH testify to critical gaps. The lack of specialized MH spaces, and abdication by, or limited discharge of duties and funds from government apparatuses have meant minimal housing support, employment assistance and other safety nets. Combined with the carceral justice system, this has resulted in many persons with mental illness being homeless, or in jail.[23]
Further, notions of “community” are themselves vague. Is community to be found in public spaces? families? neighbourhoods? workspaces? Community MH is reflected mainly in day care centers, community MH clinics or services, and health workers, while actual social support networks are often missing. Years of exclusion and stigma, with mental illness popularly associated with violence and danger, mean that living within mainstream communities has, for many, been vexed. (While public perception is that persons with mental illness perpetuate violent crimes, research bears out that they are more likely to be victims of such crimes.[24])
legacies, and passing as normal
Community or public spaces can, then, be hostile, perpetuating violence, discrimination, and stigma. The legacy of marking, removing, confining those who disrupt social norms means that expressing distress, or one’s gender, class or non-conforming behaviour, may lead to exclusion in public transport, workspaces, neighbourhoods. Attempts to “pass” or look “normal” can be difficult, due to markers such as twitching caused by medication, different time patterns because of lack of work, unconventional dress.[25] Public spaces can prove especially hard to negotiate for those who transgress as a result of their gender, sexuality, or other marginalizations – which often have a domino effect on the transgressor’s access to education, employment and healthcare services.[26]
We may understand these histories of exclusion and incarceration of people with mental illness, and the perception that people who are unproductive, or queer, are threats to the social order, as a kind of “moral panic”: ‘A condition, episode, person or group of persons emerges to become defined as a threat to societal values and interests; its nature is presented in a stylized and stereotypical fashion by the mass media; the moral barricades are manned by editors, bishops, politicians and other right-thinking people; socially accredited experts pronounce their diagnoses and solutions; ways of coping are evolved or (more often) resorted to; the condition then disappears, submerges or deteriorates and becomes more visible.’[27] In this context, the influence of mainstream morality on psychiatric treatment, which then encourages “passing”, is not surprising. Moral panic may stay in collective memory or have long-term legal, social, political repercussions. The gay or trans panic legal defenses in America, racially biased murders of black men, and police killings of persons with mental illness in public spaces are all emblematic of an ingrained moral panic.
While community MH might reside in different spaces, the influences of the asylum and psychiatry operate in mainstream spaces as well as homes, hospitals, workspaces, systems of transport. What, then, does recovery or cure look like? An absence of distress? Or distress that cant be singled out? Are there community spaces where passing or invisibility may not be required for safety? As significantly, are there MH spaces that offer counter-narratives to legacies of the asylum?
challenging legacies
MH has, in the past few decades, been moving out of brick-and-mortar institutions, and adapting to less overtly clinical community spaces. And yet, we must be cautious not to replicate, in the newer sites of mental distress and care, the old top-down biomedical approaches and power hierarchies of the asylum, obscured by the rhetoric of community and deinstitutionalization. One way to challenge the likely reproduction of asylum scripts is to engage with sites of such counter-narratives and not only shift the discourse from the biomedical to the psychosocial, but also alter the spatiality of MH – letting it be conceived of in multiple dimensions and take on many meanings. At the center of this new narrative is the individual – no longer the subject / object of the discipline of MH, but as the narrator of their own lived experience. The aim of constituting counter-narratives as a specific “site” is not to do away entirely with more traditional understandings but to create an expanded ecosystem of not just institutional frameworks, but also coalitions across disciplines, communities, and movements.
It may be helpful to think of a space not only as a demarcated physical area, but also as abstract. Which is not to suggest that it exists only theoretically, but rather as something allowing for various kinds of embodiment and meaning – not necessarily bound by the walls of an institution, or by the pillars of established approaches. An online support group for people with disabilities is, for instance, an abstract space – a possible alternative to a physical space with limited accessibility. Art therapy is abstract in that it often exists outside both, designated clinical spaces and mainstream biomedical practice. Peer support networks are abstract spaces, too, based on the intangible function of being a peer who shares a particular location, and uses the shared experience and relationality as the foundation for support that fills a gap in existing MH systems.
Such spaces can challenge the linear, ableist, and sometimes carceral approaches in MH practice. They can counter the belief that an officially designated and controlled space is necessary. They also critique the trajectory of MH, distress, and healing in the “legitimate spaces”, centering lived experience over pathology. In the mainstream sphere, for mental illness / distress that is either chronic, lifelong, or recurring, the approach always consists of diagnosis <-> prognosis <-> intervention. The intervention is meant to correct an inherent deficit or “abnormality”, thereby leading to “recovery”. There is no conception of what MH might mean outside of these rigid parameters, but abstract spaces expand on this limited interpretation, letting us think about MH as a series of practices, associations, coalitions, support networks and systems that collectively contribute to a person’s well-being. Traditional medical power / authority is displaced, creating room for an individual to express what they see as ideal outcomes, articulate their interpretation of their own experience, and make decisions about what kind of support best suits their needs – making for a more holistic and inclusive space.
identity as a site for mental health
Since community-led interventions hold the potential to deinstitutionalize and diversify the field of MH, it is important to understand just where communities come together. Identities gain significance here: several community-based, civil rights movements come from shared identity spaces, often with shared lived experiences and marginalizations. We need to acknowledge identity as a site where distress and conflict can occur, due to lack of resources, discrimination, historical disenfranchisement; and that these very sites of identity are where individuals seek solidarity, form support networks, engage in advocacy and shared dissent. Whether persons come from queer / trans identities, marginalized religious identities, or communities formed through shared experiences of chronic illness or disability, such identities sharply reveal how broader power equations may affect people’s mental health and well-being, as well as access to MH resources. Perceiving MH and distress in terms of privilege and oppression also lets us question whether the most visible MH services and narratives are also the most privileged ones. In challenging mainstream conceptions of MH, counter-narratives from the margins become a valid critique of the power systems that may be reproduced within that mainstream.
It is crucial to acknowledge histories, power structures, and the complicity of psy-disciplines in propounding and propagating the “normal”. While the idea of community MH may lead to closures of asylums, the violent heritage of the clinical continues to operate in the carceral systems, in public spaces hostile to the homeless, and mainstream community spaces that subscribe to the clinically defined “normal”. We must look to other spaces, different sites, to examine our approaches more critically, even as we strive to deinstitutionalize MH. To counter the biases that were the foundation of the clinic, we must look constantly to spaces that have been engaged in MH support outside of the clinic, and be guided by their value systems.
Amalina Kohli Dave is a mental health activist and user-survivor who has organized queer MH discussion groups, and co-hosted a series of workshops about MH in theatre. She has also started support groups for people with chronic illness.
Raj Mariwala is Director, Mariwala Health Initiative.
[1] McAvoy J. (2014) Psy Disciplines. In: Teo T. (eds) Encyclopedia of Critical Psychology. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-5583-7_611
[2] Scull, A. T. (1981). Madhouses, mad-doctors, and madmen: The social history of psychiatry in the Victorian era. Philadelphia, Pa.: University of Pennsylvania Press.
[3] Arnold, C. (2009). Bedlam: London and its mad. London: Pocket Books.
[4] Scull, A. (2016). Madhouses and Mad-Doctors. In Madness in civilization: A cultural history of insanity from the Bible to Freud, from the madhouse to modern medicine. Princeton, NJ: Princeton Univ. Press.
[5] Porter, R. (2004). Madmen: a social history of madhouses, mad-doctors and lunatics. London: Tempus.
[6] Science Museum. (2018, June 13). A Victorian Mental Asylum. https://www.sciencemuseum.org.uk/objects-and-stories/medicine/victorian-mental-asylum
[7] Foucault, M. (1965). Madness and civilisation. New York: Vintage.
[8] Historic England. (2017, April 3). From Bethlehem to Bedlam - England’s First Mental Institution | Historic England. https://historicengland.org.uk/research/inclusive-heritage/disability-history/1050-1485/from-bethlehem-to-bedlam/
[9] Ray, L. (1981). Models of madness in Victorian asylum practice. European Journal of Sociology / Archives Européennes De Sociologie / Europäisches Archiv Für Soziologie, 22(2), 229-264. Retrieved August 7, 2020, from www.jstor.org/stable/23999303
[10] Davar, B. Disabilities, colonisation and globalisation: How the very possibility of a disability identity was compromised for the ‘insane’ in India, Davar, B. In Spandler, H., & Anderson, J. (2015) Madness, Distress and the Politics of Disablement (1st ed., pp. 215–227). Policy Press.
[11] Amdur, M. K., & Messinger, E. (1939). Jean-Etienne-Dominique Esquirol. American Journal of Psychiatry, 96(1), 129–135. https://doi.org/10.1176/ajp.96.1.129
[12] Mishra A, Mathai T, Ram D. History of psychiatry: An Indian perspective. Ind Psychiatry J. 2018;27(1):21-26. doi:10.4103/ipj.ipj_69_16
[13] Ebert, A., & Bär, K. J. (2010). Emil Kraepelin: A pioneer of scientific understanding of psychiatry and psychopharmacology. Indian journal of psychiatry, 52(2), 191–192. https://doi.org/10.4103/0019-5545.64591
[14] Kawa, S., Giordano, J. A brief historicity of the Diagnostic and Statistical Manual of Mental Disorders: Issues and implications for the future of psychiatric canon and practice. Philos Ethics Humanit Med 7, 2 (2012). https://doi.org/10.1186/1747-5341-7-2
[15] Science Museum. (2018, June 13). A Victorian Mental Asylum. https://www.sciencemuseum.org.uk/objects-and-stories/medicine/victorian-mental-asylum
[16] Charland, L. (2011). Moral treatment in 19th and 18th century psychiatry. In A. Rudnick & D. Roe (Eds.), Serious Mental Illness: Person-Centered Approaches (Patient-centered Care) (1st ed., pp. 1–13). CRC Press.
[17] Scull, A. (2016). Madness in Civilization: A Cultural History of Insanity, from the Bible to Freud, from the Madhouse to Modern Medicine (Reprint ed.). Princeton University Press.
[18] Feldman, J. M. (2012). History of Community Psychiatry. Handbook of Community Psychiatry, 11–18. https://doi.org/10.1007/978-1-4614-3149-7_2
[19] Dave, A. K., Mariwala, R. (2018, September). ReFrame: Funding Mental Health (No. 1). Mariwala Health Initiative. https://mhi.org.in/media/insight_files/MHI_Progress_Report_DIGITAL.pdf
[20] Novella, E.J. (2010). Mental health care and the politics of inclusion: a social systems account of psychiatric deinstitutionalization. Theor Med Bioeth, 31: 411-427.
[21] Thornicroft, G., Deb, T., & Henderson, C. (2016). Community mental health care worldwide: current status and further developments. World psychiatry : official journal of the World Psychiatric Association (WPA), 15(3), 276–286. https://doi.org/10.1002/wps.20349
[22] Campbell, P., and Rose, D. (2011). “Action for change in the UK: Thirty years of the user/survivor movement,” in The SAGE Handbook of Mental Health and Illness, eds D. Pilgrim, A. Rogers, and B. Pescosolido (London: Sage), 452–470. doi: 10.4135/9781446200988.n22
[23] Priebe, S., Badesconyi, A., Fioritti, A., Hansson, L., Kilian, R., Torres-Gonzales, F., Turner, T., & Wiersma, D. (2004). Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ, 330(7483), 123–126. https://doi.org/10.1136/bmj.38296.611215.ae
[24] Varshney, M., Mahapatra, A., Krishnan, V., Gupta, R., & Deb, K. S. (2015). Violence and mental illness: what is the true story? Journal of Epidemiology and Community Health, 70(3), 223–225. https://doi.org/10.1136/jech-2015-205546
[25] Estroff, S. E. (1981). Psychiatric deinstitutionalization: A sociocultural analysis. Journal of Social Issues, 37(3), 116–132. https://doi.org/10.1111/j.1540-4560.1981.tb00832.x
[26] Shah, C., Merchant, R., Mahajan, S., & Nevatia, S. (2015). No Outlaws in the Gender Galaxy. Zubaan Books.
[27] Cohen, S. C. S. (2002). Folk Devils and Moral Panics: Thirtieth Anniversary Edition:2nd (Second) edition. Taylor & Francis, Inc.