Interrogating the Cut + Paste of ‘Recovery’
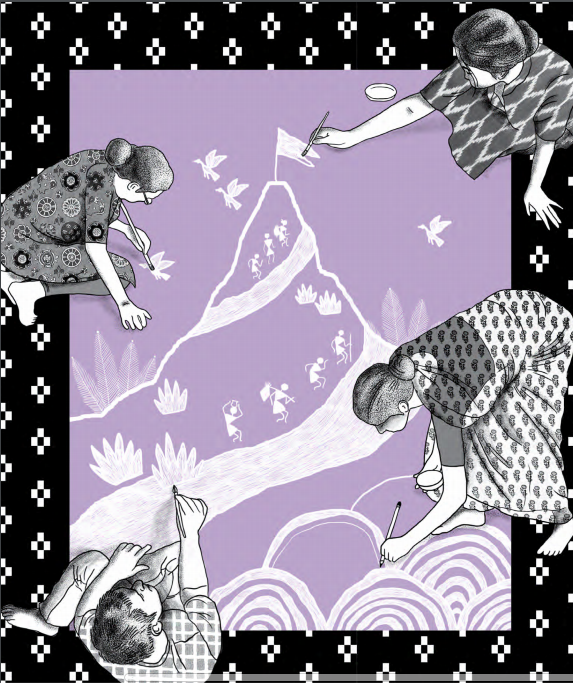
Experts by experience build locally valid definitions
contexts for recovery
This article challenges received wisdom on existing concepts of ‘recovery’ from mental suffering and demands that people’s voices ought to be central to future policy, clinical care, and applied research. ‘Recovery’ is a concept that proposes we can live fulfilling lives despite our suffering. It has been embraced by people affected by mental distress in high-income countries (HICs). Indeed, current ideas of recovery have emerged from the particular histories of mental health service user movements in HICs . This represents a significant shift in the idea of recovery, from being about symptom remission to suggesting a process – a “journey of change” – for the individual.
In the Indian context, whilst it has been the subject of much discussion in the mental health field, there has been limited focus on recovery in formal mental health services. The idea of recovery has been welcomed, although the frameworks for addressing this have been adopted rather uncritically from high-income settings. There are still almost no social recovery tools developed for Indian contexts, or together with affected persons. Data on what recovery means to Persons with Psychosocial Disabilities (PPSD), carers, and local communities, is crucial to ensuring that India’s community mental health programmes embed locally valid understandings. How social recovery takes place, what aspects are central (having friends, or paid work, or being able to have fun), the measures of social recovery, and the types of support that people with mental health problems would like, all vary in different contexts.
defining “recovery”
In the early 2010s, we noted the emergence of the term “recovery” in Indian psychiatric circles and in India’s new mental health policy. This led us to ask two questions:
- What is the distinctive history of this concept?
- How relevant is it to the Indian context?
In parallel, Mathias, in setting up a community mental health programme called Burans in Uttarakhand, faced challenges in operationalizing conventional western recovery tools. These tools were often inaccessible to people due to the way they were structured, and the lack of cultural validity. Both the underpinning ideas of recovery, and the domains embedded in these tools, seemed to hold little meaning or relevance to the lives of the PPSD with whom the Burans team was working.
These challenges resulted in a one-year pilot project* to develop a pictorial recovery tool relevant to the north Indian context. A core idea underpinning this work was the importance of identifying “Indian vernacular concepts of ‘recovery’, their cognate and embodied equivalents.” Our effort was to operationalize this in the context of a short project cycle. We began by holding workshops, and meetings with PPSD and carers – all of whom were “experts by experience”. We used participatory methods, including storytelling, discussing photographs drawing pictures, and focus group discussions to better understand local meanings of recovery, and generate valid domains for the tool. Two key Hindi-language terms on which the group agreed were swasth rehna (remaining in good health) and theek hona (to get well). The group named a resulting tool Swasthya Labh Saadhan (recovery tool for health). The aspects of recovery that emerged emphasized the importance of a person’s role as an active member of the community and family, being spiritually engaged, and contributing to the family – perspectives that are missing in most western recovery tools.
A local artist created pictures representing domains of recovery, an important adaptation for settings where literacy may be a limiting factor. The use of this co-developed how do we develop supportive community environments? A central limitation in our research was that we primarily addressed individual narratives and domains of recovery. While important, this can serve to obscure the structural issues that shape well-being and marginalization — which may be mental health recovery tool among a pilot group of 26 people with severe mental illness led to improved mental health, and generated local conversations around recovery between lay workers and PPSD .
*This project is funded by Economic and Social Research Council Impact Acceleration Account for The University of Edinburgh.

Conceptions of what recovery means for community members in the project area
translating to practice, policies and communities
Several questions that emerged from this work have relevance for India’s community mental health services: what does “recovery” mean in indian contexts? If we are to develop services that are locally valid, it is crucial to embed a participatory process of identifying domains of recovery in each context. Conceptions of what recovery means may widely vary between policy makers, clinicians, PPSD and carers. These differences are yet to be understood in this context, but are crucial for culturally valid visions of recovery to emerge. Independent of services, more research, including analysis of existing qualitative and ethnographic data, is needed to understand trajectories of recovery as well as the intersections of psychosocial disabilities with other forms of marginality (such as gender, religion and caste). This is crucial, given India’s cultural and social diversity. how can services better embed co-production with “experts by experience”? The depth of our approaches was limited by project time. A recent paper by service user/survivor researchers highlights the unequal power relationships that accompany co-production in mental health care. In our research, we soon became aware of these power differentials between researchers/mental health workers, and people with psychosocial disabilities and carers. A first step towards mitigating these inequalities would be to ensure that the voices of “experts by experience” are heard and dedicated in planning, developing and delivering community mental health care in the country. This would, however, be only a start – the more important concern is with how diverse voices can truly inform the priorities and directions of mental health care systems? People-centred approaches to health systems offer a useful framework. These approaches recognize the centrality of individual, family and community perspectives, conceptualize them as participants and beneficiaries in the health system, and advocate for organizing health services around people’s needs.
how do we develop supportive community environments?
A central limitation in our research was that we primarily addressed individual narratives and domains of recovery. While important, this can serve to obscure the structural issues that shape well-being and marginalization — which may be beyond individual control and that limit service user involvement. For example, we know very little about how social inequalities such as caste, identity intersect with mental health. In thinking about recovery, research and practice must be informed by an understanding of the wider social and material forces that shape suffering, including gender, age, social class, and caste.
“The important concern is how diverse voices can truly inform the priorities and directions of mental health care systems.”
Authors
Dr. Sumeet Jain is Senior Lecturer in Social Work at The University of Edinburgh. Current research in South Asia examines mental health ‘innovations’; local approaches to ‘recovery’; the role of community health workers in delivery of mental health care; and mental health, marginality and social exclusion.
Dr. Kaaren Mathias is the Mental Health Programme Manager, Emmanuel Hospital Association (www.eha-health. org) and Project Director of Burans in Uttarakhand (https://projectburans. wixsite.com/burans). Research interests include models for community mental health, youth resilience, participation, exclusion and inclusion of people with mental distress, gender, equity, and health system strengthening.
Clément Bayetti is a Doctoral Student at University College London (UCL), UK and an Adjunct Faculty at Washington University, St. Louis, USA. His research explores the process through which psychiatry students in India acquire professional identity and how this shapes clinical encounters and outcomes.
Dr. Sushrut Jadhav is a street psychiatrist working for homeless people. He is a clinician anthropologist and Clinical Associate Professor, Cross-cultural Psychiatry, University College London. Dr Jadhav is currently engaged in field testing cultural psychological therapy for caste mediated distress.